First reported use of a TCI™ Articulating Introducer with Video Laryngoscopy in Patients with Cervical Spine Immobility due to Instability of fusion. Three Successful First Pass Intubations.
In preparation for publication.
January 2020
Guillermo Navarro, M.D.* and Rubén Allori, M.D. Hospital de Emergencias
Clemente Alvarez Rosario, Argentina
Loren Knecht, MD. Assistant Professor, University of Utah SOM,
Salt Lake City UT, USA
Airway management in patients with cervical injury can be challenging because of the need to limit spine motion during tracheal intubation in order to minimize the risk of neurologic damage. Neurological complications can occur in this setting. (Muckart 1997) The Ideal intubation technique in this setting is unknown. (Hagberg 2014)
In addition, cervical immobility due to fusion can also present challenges during intubation.
Awake fiberoptic bronchoscopy (aFOB) may be used for intubation and has traditionally been the intubation technique of choice. However, a FOB’s usefulness in the acute setting can be limited by availability, training, uncooperative patients and soiled airways. (Holmes 2019)
Other techniques may be used safely as well. Direct laryngoscopy (DL) with In line stabilization (ILS), video laryngoscopy (VL) with ILS, blind nasal intubation, and lighted stylets have all been used and reported as safe. A recent study demonstrated VL as the leading choice at one high volume trauma center in the US. (Holmes 2019)
We report a series of 3 intubations performed successfully on the first pass in patients with unstable cervical spine pathology which limits the ability to flex or extend the neck during intubation. A Total Control Introducer ™ (TCI™) (Through The Cords, LLC, Salt Lake City Utah) was used in conjunction with a video laryngoscope an articulating introducer to intubate each smoothly on the first pass. The TCI™ can be dynamically shaped while moving through the upper airway and into the trachea. Once in the trachea, a zonal depth system, printed on the shaft of the introducer, provides intuitive depth control at the level of the glottis.
We believe these are the first reported uses of the TCI™ in the setting of cervical immobility due to fusion or instability.
Consent for photos and publication were obtained from all patients.
Case 1 (photo series 1)
A 36 year old male with a traumatic unstable c-2 fracture was scheduled for surgery. Standard ASA monitors were placed on the patient. The patient was pre oxygenated with 100% Oxygen and induced with 100 mcg of fentanyl, 150mg of propofol, and 50mg of Rocuronium. Once neuromuscular relaxation was obtained, the front of the C collar was kept in place to maintain ILS. A Glidescope™ with a hyperangulated blade was used to obtain a grade 1 view of the glottic opening. A TCI™ articulating introducer was then placed into the mouth along the right side of the video laryngoscope blade and maneuvered into the trachea, taking advantage of its ability to be dynamically shaped. The tip of the introducer was straightened, using the trigger of the pistol grip handle, and advanced into the mouth along the right side of the VL blade Once in the view of the VL, the tip of the introducer was anteflexed, and advanced to the vocal cords. The tip was then retroflexed posteriorly and smoothly advanced over the glottis, through the vocal cords, and into the trachea until the green depth band was next to the vocal cords. The handle of the TCI™ was removed. The ETT was then railroaded over the introducer and into the trachea taking care to control the depth of the introducer by keeping the green zone at the vocal cords throughout the procedure. Once the ETT was properly positioned in the trachea, the TCI™ was removed out the back of the ETT, leaving the ETT in place in the trachea. Endotracheal intubation was confirmed with CO2
and bilateral auscultation. Intubation took place smoothly on the first attempt without complications.
Case 2 (photo series 2)
A 41 year old male with a traumatic unstable lower cervical fracture and dislocation was scheduled for surgery. Standard ASA monitors were placed on the patient. The patient was pre-oxygenated with 100% Oxygen and induced with 100 mcg of fentanyl, 150mg of propofol, and 50mg of Rocuronium. Once neuromuscular relaxation was obtained, the front of the C collar was removed. Care was taken to keep the neck from moving but no ILS was applied. A Glidescope™ with a hyperangulated blade was used to obtain a grade 1 view of the glottic opening. A TCI™ articulating introducer was then placed into the mouth along the right side of the video laryngoscope blade and maneuvered into the trachea, taking advantage of its ability to be dynamically shaped. The tip of the introducer was straightened, using the trigger of the pistol grip handle, and advanced into the mouth along the right side of the VL blade. Once in the view of the VL, the tip of the introducer was anteflexed, and advanced to the vocal cords. The tip was then retroflexed posteriorly and smoothly advanced over the glottis, through the vocal cords, and into the trachea until the green depth band was next to the vocal cords. The handle of the TCI™ was removed. The ETT was then railroaded over the introducer and into the trachea taking care to control the depth of the introducer by keeping the green zone at the vocal cords throughout the procedure. Once the ETT was properly positioned in the trachea, the TCI™ was removed out the back of the ETT, leaving the ETT in place in the trachea. Endotracheal intubation was confirmed with CO2 and bilateral auscultation. Intubation took place smoothly on the first attempt without complications.
Case 3 (photo series 3)
A 27 year old female status post anterior and posterior cervical fusion was scheduled for surgery. Her exam was notable for total neck immobility, mouth opening of 1.7 cm, and a hard C collar in place. Standard ASA monitors were placed on the patient. The patient was pre-oxygenated with 100% Oxygen and induced with 100 mcg of fentanyl, 150mg of propofol, and 50mg of Rocuronium. Once neuromuscular relaxation was obtained, the front of the C collar was left in place. A Glidescope™ with a hyperangulated blade was used to obtain a grade 1 view of the glottic opening. A TCI™ articulating introducer was then placed into the mouth along the right side of the video laryngoscope blade and maneuvered into the trachea, taking advantage of its ability to be dynamically shaped. The tip of the introducer was straightened, using the trigger of the pistol grip handle, and advanced into the mouth along the right side of the VL blade Once in the view of the VL, the tip of the introducer was anteflexed, and advanced to the vocal cords. The tip was then retroflexed posteriorly and smoothly advanced over the
glottis, through the vocal cords, and into the trachea until the green depth band was next to the vocal cords. The handle of the TCI™ was removed. The ETT was then railroaded over the introducer and into the trachea taking care to control the depth of the introducer by keeping the green zone at the vocal cords throughout the procedure. Once the ETT was properly positioned in the trachea, the TCI™ was removed out the back of the ETT, leaving the ETT in place in the trachea. Endotracheal intubation was confirmed with CO2 and bilateral auscultation. Intubation took place smoothly on the first attempt without complications.
Discussion
The Ideal intubation technique for managing patients with unstable cervical spines has yet to be established. ILS is recommended to protect the patient from injury to the spinal cord. ILS minimizes the motion of the cervical spine during intubation; however, immobilization of the cervical spine makes intubation challenging as airway geometry is fixed.
Greenland et al. described 2-curves dividing the airway passage into a primary (oro-pharyngeal) curve and secondary (pharyngo-glotto-tracheal) curve. Successful intubation requires solving both curves. (Greenland 2010) With ILS in place, the solution cannot be to flatten or modify the curves of the airway.
The VL can look around the primary curve providing a view of the glottis, mitigating the problem of visualization. It is critical to understand that by looking around the corner, the lower mandible and head are not lifted, and the primary and secondary curves are left largely intact. Because these curves are not flattened during VL, the endotracheal tube (ETT) must be delivered around the two intact corners. The serpentine pathway created with ILS and VL can make ETT delivery particularly challenging.
One solution to solving both the primary and secondary curves during intubation is the ‘combined technique’ or ‘hybrid technique’ which utilizes VL for visualization of the glottis and a FOB for navigation into the trachea and delivery of the ETT. (Chung 2018) The VL is placed into the mouth and a view of the glottis is obtained. A FOB is pre-loaded with an ETT and introduced in the airway alongside the VLS. The FOB is then maneuvered into the airway taking advantage of the ability to dynamically control the curvature of the FOB tip and distal shaft; providing precision maneuvering into the trachea. Finally, the ETT is pushed down the FOB shaft and into the trachea.
A combined or hybrid technique in which VL is an interesting option as it is reported to have a high first pass rate.
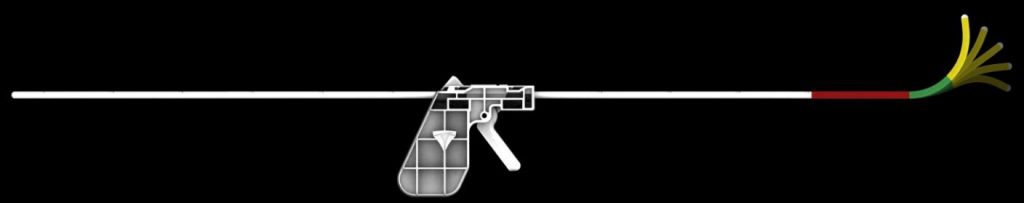
We present a series of thee patients with unstable cervical spines that were intubated using a VL for visualization of the glottis and a new introducer, the TCI™, which possesses a flexible shaft and a dynamically shapeable tip. (See figure 1) Dynamic tip control offers the ability for the operator to both antiflex and retroflex the introducer tip while maneuvering into the trachea. Once in the trachea, the control handle can be removed, and the endotracheal tube railroaded over the introducer and into the trachea using Seldinger’s technique.
All patients in this series were intubated smoothly on the first pass while the cervical spine was held immobile with ILS or a hard cervical collar.
Modification of the ‘combined’ or ‘hybrid’ technique by using a TCI™ in place of the FOB may offer several advantages over classic ‘combined’ or ‘hybrid technique’. First, the TCI™ possesses a flexible shaft that is stiffer than a FOB. The shaft is stiff enough to both advance the TCI™ using a single hand on the pistol grip handle and then act as a guide, without bending excessively, while advancing the ETT over the introducer. At the same time, it is flexible enough to conform to the upper airway and trachea, increasing maneuverability and potentially reducing the risk of trauma. Second, the intuitive depth control system on the shaft allows depth to be managed at the level of the vocal cords without looking away from the screen.
Furthermore, the modified combined or hybrid technique using a TCI™ seems easy to learn. In this case, the provider was remotely trained via screen share over the internet, practiced on an airway manikin, used the TCI™ on a normal airway in a patient, and then carefully self-advanced into more challenging airways. The airways reported in this paper are numbers 3,4 and 6 of his case series.
In theory, VL for visualization combined with a dynamically shapeable introducer offers answers to the challenges of intubation with minimal cervical spine motion. Though not rising to the level of evidence, there are some interesting clues available in the literature. (Holmes 2018, Lenhardt 2014)
A recent case series from a large high-volume trauma center in the US demonstrated that VL was the most common technique used making up over half of all intubations.
Two hundred fifty-two patients were included; VL was the most frequent initial airway management technique used (49.6%). Asleep FOB was commonly performed alone (30.6%) or
in conjunction with VL (13.5%). Awake FOB was rarely performed (2.3%), as was direct laryngoscopy (2.8%). (Holmes 2018)
Interestingly, VL/FOB were used together in 13.5% of cases achieving a 100% (23/23) first pass rate. This hybrid or combined technique essentially uses VL to provide visualization and FOB to provide a dynamically shapeable introducer for maneuvering into the trachea.
Additionally, VL/FOB was successfully used as a rescue technique in 6 cases after first attempt failure with VL (1), FOB (5). Lenhardt also achieved a 100% success rate for rescue after VL first pass failure in his study.
Though neither is conclusive, together they offer a tantalizing glimpse into what may be possible when a video laryngoscope is used to look around the primary curve to solve visualization, and dynamically shapeable introducer is used to maneuver around the primary and secondary curves of the airway.
Is VL for visualization combined with a dynamically shapeable introducer a better technique for intubating patients with unstable cervical spines? In theory, VL for visualization, combined with a dynamically shapeable introducer, offers answers to the challenges of intubation with minimal cervical spine motion. Currently, the literature cannot provide an answer.
Further studies of various intubation techniques to better understand associated variations of visualization, ease of tube delivery, learning curves, provider mental task load, and success rates are needed to test this theory.
Conclusion
We report the first case series of airway management with a VL and the TCI™, a dynamically shapeable articulating introducer, in the setting of unstable cervical spines. All patients were intubated smoothly and successfully on the first attempt with no complications.
Photo series case 1





Photo Series Case 2



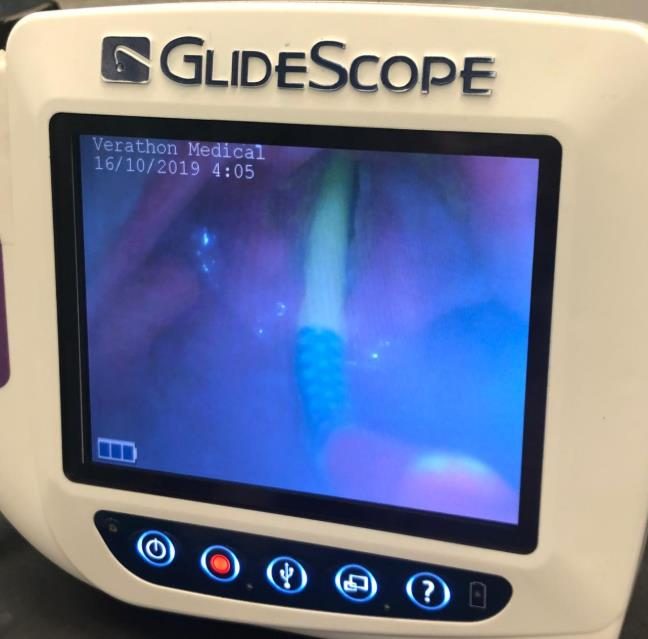
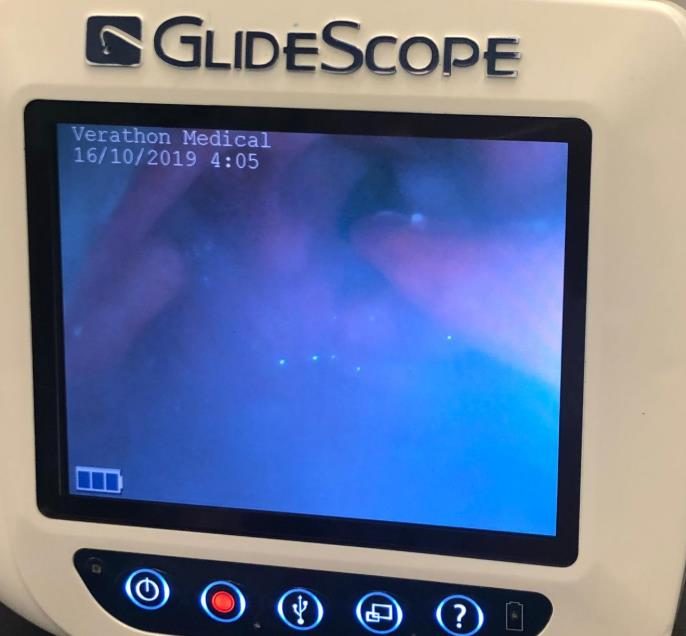
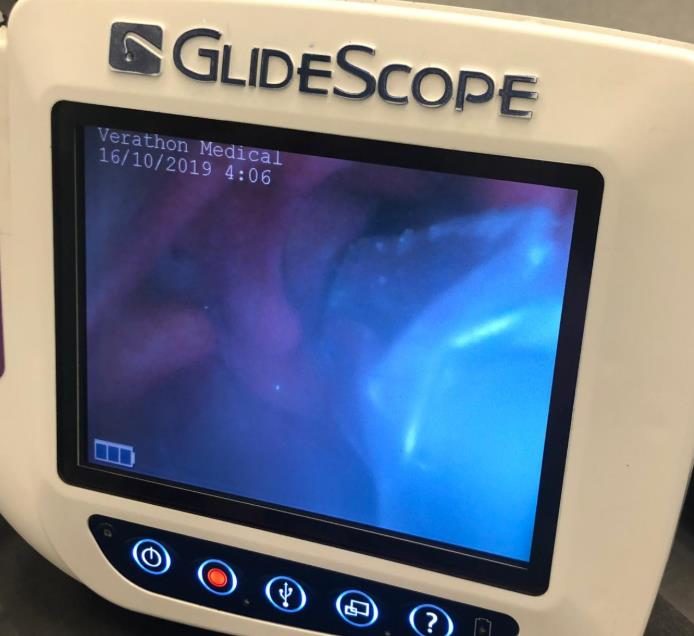

Photo Series Case 3





Figure 1
References
Hagberg CA, Kaslow O. Difficult airway management algorithm in trauma updated by COTEP. ASA Monitor. 2014;78:56–60.
Muckart DJJ, Bhagwanjee S, Van der Merwe R: Spinal cord injury as a result of endotracheal intubation in patients with undiagnosed cervical spine fractures. Anesthesiology 1997; 87:418-20.
Michael G. Holmes, MD,* Armagan Dagal, MD, FRCA,† Bryan A. Feinstein, BA,* and Aaron M. Joffe, DO, FCCM† Airway Management Practice in Adults With an Unstable Cervical Spine: The Harborview Medical Center Experience August 2018 • Volume 127 • Number 2
Lenhardt, MD,*† Mary Tyler Burkhart, MD,* Guy N. Brock, PhD,‡ Sunitha Kanchi-Kandadai, MD,* Rachana Sharma, MD,* and Ozan Akça, MD, FCCM*† (Anesth Analg 2014;118:1259–65)
K. B. Greenland, M. J. Edwards, N. J. Hutton, V. J. Challis, M. G. Irwin, J. W. Sleigh, Changes in airway configuration with different head and neck positions using magnetic resonance imaging of normal airways: a new concept with possible clinical applications, BJA: British Journal of Anaesthesia, Volume 105, Issue 5, November 2010, Pages 683–690, https://doi.org/10.1093/bja/aeq239